The Other Side
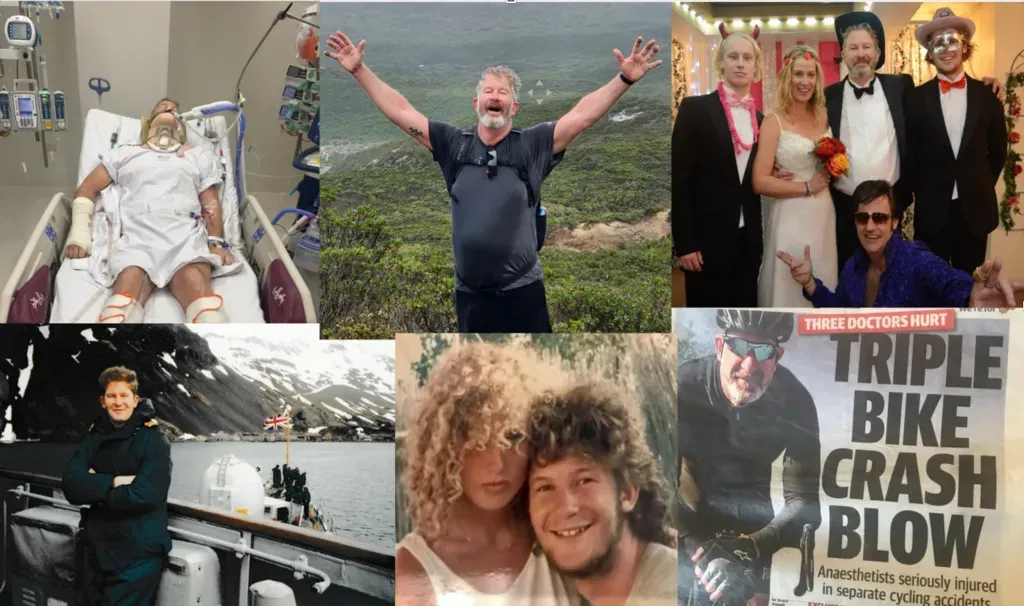
ON 16 SEPTEMBER 2018 my medical career ended. It wasn’t that I made a terrible mistake with a patient’s care or falsified my tax return. I hadn’t suffered an epiphany of self-doubt in the face of the tragedy and sadness that so often colours our lives as doctors. I wouldn’t even say that I had found the working pressures and expectations too onerous to bear any more, growing accustomed as we all must, to a professional life of clinical crises and administrative torment. In fact, I’d probably come to take my charmed life in Western Australia for granted having largely figured out how the patients, the people and the politics stuff really worked.
I think that I felt that I was at the peak of my powers, widely qualified across medicine, critical care and anaesthesia, working both publicly and privately. As the state’s leader of Donate Life, donor numbers had almost tripled in six years and no one was more surprised than me that I was the longest-ever serving medical director. Unfortunately it turns out that pride really does comes before a fall. To be precise, on a damp chilly morning, descending the steep and slippery road into the Victorian coastal town of Apollo Bay, I cycled head-on into a street sign at 65 km h.
I don’t remember any of the bad stuff, the broken neck and shattered jaw, the partial scalping and the torn off ear, the crushed chest and multiple lumbar fractures. I missed the worst of the anxiety and pain, ventilated and restrained for a week while my family held a vigil at my bedside. I also missed the fear and the distress, the sleepless nights and the over-the-phone consents for stabilising trauma surgery that I inflicted upon them. Once I finally awoke in the intensive care unit many days later, my wonderfully gentle wife Anita repeatedly had to explain to me that I was a patient and not the on-call consultant.
Even after I had escaped the critical care and trauma wards, my befuddled brain still defaulted to familiar behaviours, wandering around the rehab hospital TV room in my pyjamas, examining other’s wounds and drip sites on my daily “ward round”. Afterwards, mentally exhausted, I would then fall asleep watching another Netflix series that I wouldn’t remember.
In time honoured medical tradition, I even tried to cheat on my cognitive assessments by plotting with my dear brain-tumor roommate to memorise the questions that he was asked. Sadly I couldn’t remember any of his prepared answers and failed miserably. It’s a long journey back to medical expertise when you can only recite two of a list of 15 words that you’re meant to remember. Having returned from Melbourne six weeks after the crash, rehabilitation at Fiona Stanley Hospital in Perth was confronting and upsetting. The fight to recover drove a bewildering mix of emotions.
I seemed to be the only one in clinic not in a wheelchair and for that I felt terrible guilt and perverse regret. I was ashamed because I even had to make up stories foreach of my amazing carers, just to allow me to recall their names. Michelle (“two-little-legs-runner”) the occupational therapist cared for me with such patience and kindness. (“Whiffy”) Miffy at the state head injury unit was all optimism and empathy in the face of my stream of tangential consciousness and bitter rage. Times had now changed. I was suddenly afraid of uncertainty, wary of my explosive, irrational anger and reckless nature. The diffuse axonal injuries had left my personality peppered with multiple micro-haemorrhagic holes and through them the irrationality could uncontrollably flow out. I would cry repeatedly during our hours together and each would sit quietly and wait for the emotional squalls to pass. In between showers of tears I would rage and laugh, wandering without embarrassment or insight across a whole range of unrelated personal topics. My rehab consultant told me bluntly, when we first met unscheduled in a corridor, that she didn’t know if I would ever work again. I was so angry and upset, having fought irrationally hard with only that single outcome in mind, that it wasn’t until the rush hour train journey home that I calmed down enough to blub embarrassingly once more.
How could any of the rehab team know whether I was fit to practice? Who even knew what us gassers did?
“Exhaustive knowledge of human physiology?”
“Precise dosing of dangerous and complicated drugs?”
“Hours of intense concentration?
”All that sounded very challenging but nothing like what I did as a senior clinician.
It was only as the time came closer to reboot my expertly crafted 80s operating theatre playlists that the reality began to dawn. Physically, my “Jeff Bridges” beard now hid the metalwork in my chin and only the subtle neck and hand scars betrayed the plates and screws holding my head and hands on.
I looked pretty normal, long hair and all. As D-day of my return to work approached, through repeated sleepless nights, I was forced to admit to myself that I was afraid of the huge responsibility that us anaesthetists bear and realised how often I would have to hide my own anxieties to facilitate others doing their jobs. An anaesthetist’s lot is not to take centre stage but to quietly keep everything in order. Early on in our relationship, I tried to tell my brilliant private surgical partner of my concerns for a particular patient. “Sorry Bruce” he interrupted “I don’t want you to take this the wrong way but I’m not really interested. You know what you’re doing. I’ll just wait until you’re ready.
”His dismissal of my concerns had me livid for a moment and then just as quickly very flattered and emboldened by his trust in me. We were a great team for that very reason, that and a shared love of beer and oysters. Naturally it can be daunting to be a leader and us anaesthetists often have to step up. We are relied upon, trusted with command of the ship when the storm breaks, deliberately calm and precise. For all the time that I had fought to return to work, I had sub consciously belittled my role. I had focused upon the ease that 25 years of experience and hard graft had afforded me. “I’m only an anaesthetist” I used to dismissively say. On reflection that was true, in the same way that Donate Life’s extraordinary donor co-ordinators are “only” administrators, mere facilitators. Of course the reality is that both groups are only noticed when things go wrong, when fault needs to be attributed. That is when we have to stand up and lead. Otherwise we just sit quietly, “drinking coffee”, “playing sudoku”, crediting others with the successes and the lives saved.
"The greatest ally of the physician is time” my first medical consultant used to recite before each ward round. I remind myself of that incantation when the black dog tries to interrupt my morning ocean swim. I won’t ever anaesthetise again and that is hard to accept. I am acutely conscious that I am much luckier than other trauma victims and for that I quietly rejoice. I think that I’m finally done trying to remember what happened yesterday. I’m certain that today and tomorrow are much more important.