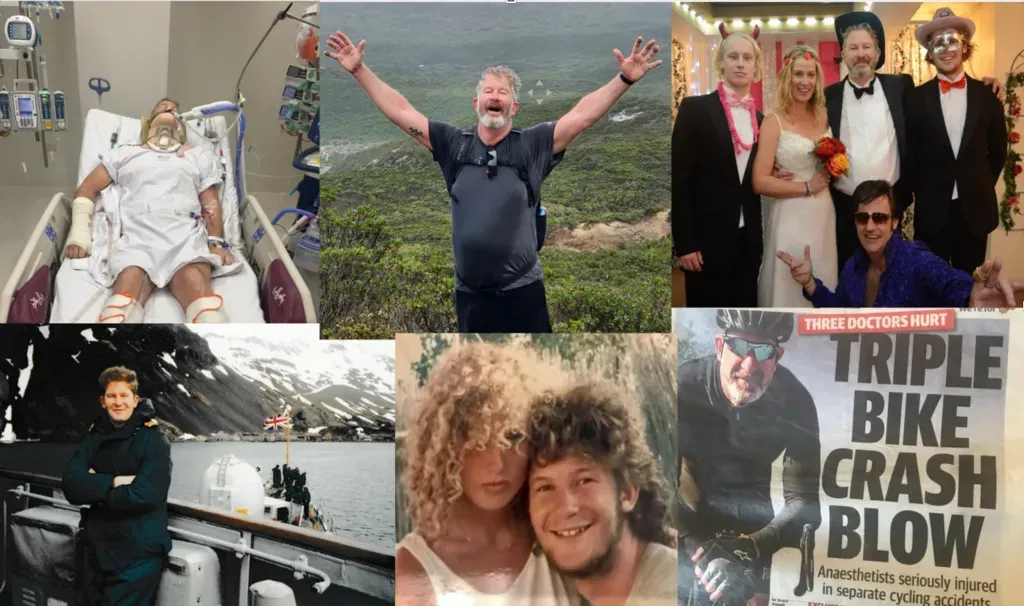
Is Rehabilitation Really Valued?
Brain Injury Rehabilitation, Funding Challenges, and the Hidden Value for Patients, -Carers, and Society
During the COVID-19 crisis, rehabilitation services were among the hardest hit. According to the Australasian Rehabilitation Outcomes Centre (AROC):
- 43% of inpatient rehabilitation services were closed or repurposed.
- 46% of outpatient rehab services shut down.
- Half of all Allied Health outpatient staff were redeployed to other areas.
This disruption exposed a long-standing truth: rehabilitation is still undervalued, underfunded, and under-recognised. Yet the science is clear — for every $1 invested in rehabilitation, $92 is returned in long-term savings (BMJ). No other sector of healthcare offers a higher return. So why does rehabilitation remain an afterthought?
Carers: The Hidden Sacrifice Behind Rehabilitation
Families of people with a brain injury understand rehabilitation better than anyone. They know it is life changing, but they also know it is all-consuming. Without structured neuro-rehabilitation, patients rarely achieve independence. Without carers, even the best rehabilitation cannot succeed.
Too often, carers sacrifice their own futures because systems do not provide enough support. They step back from careers, education, and personal ambitions to fill the gaps. But must carers carry this heavy burden forever? Or should governments properly fund rehabilitation so carers have a real choice — free from guilt, exhaustion, and impossible sacrifice?
Why Is Rehabilitation Funding So Difficult?
The challenge is political and financial. Rehabilitation costs are immediate, visible, and fall squarely within health budgets. The benefits, however, are spread across society:
- Reduced welfare dependency.
- Increased workforce participation.
- Stronger family resilience.
- Lower long-term medical and aged-care costs.
Yet Medicare and insurance rarely cover the full rehabilitation journey. Critical elements like physiotherapy, occupational therapy, speech therapy, psychology, glasses, hearing aids, home nursing, and even ambulance services often fall outside the system. Families and patients are left to fill these gaps themselves, often at great personal cost.
What’s Wrong With the Current Rehabilitation System?
Rehabilitation is not broken, but it is consistently neglected.
The challenges include:
- Slow and invisible: No TV dramas, no viral headlines, no protest marches.
- Chronic underfunding: ICU and surgery attract investment; rehabilitation receives the leftovers.
- Hidden burnout: Dedicated staff cover shortages with unpaid overtime, masking systemic cracks.
- Cultural neglect: Rehabilitation is still treated as the “poor cousin” of acute medicine.
The result? Patients wait longer, staff burn out faster, and carers shoulder more than they should.
Do We Really Value Rehabilitation Outcomes?
Traditional cost-effectiveness measures consistently undervalue rehabilitation:
- High-dependency patients often make huge functional gains, but these improvements are not captured by blunt disability scales.
- Cognition and behavioural changes — which can mean the difference between dependence and employment — are rarely measured, despite their immense economic value.
- Inpatient rehabilitation shortens total hospital stays, saving up to 150% in costs compared with acute wards.
The numbers prove it: intensive inpatient rehabilitation, combined with structured outpatient support, is one of the best investments a healthcare system can make.
The Challenge for Politicians
Governments tend to count the costs of rehabilitation in the short term but struggle to measure the benefits that flow across decades. Ministers see budgets, not people; deficits, not carers’ sacrifices; line items, not lives regained.
But rehabilitation is not a dumping ground for the chronically ill. It is the foundation of independence, recovery, and reintegration into society. If we valued outcomes honestly, we would reframe rehabilitation not as an expense, but as one of the smartest, highest-return investments in modern healthcare.
Rehabilitation is not about extending costs — it’s about reducing them while restoring dignity and giving patients, carers, and communities the chance to thrive.