“Is it OK to Cry?”
“I was better after I had cried than before – more sorry, more aware of my own ingratitude, more gentle.”
Charles Dickens. Great Expectations.
I cried quite frequently when I was working, although not in front of colleagues or patients if I could help it. Tears were a release, not an omen of imminent meltdown. I could just as easily make some uncomfortably dark joke and move on. Also, my outbursts didn’t have to specifically be caused by one of our patients. Sometimes a combination of personal life pressures and work responsibilities had me sitting in the consultant’s car park sobbing. It never occurred to me that I might be depressed or need help, since open expressions of emotion were a family trait that I never grew out of. I only recognised the ‘tear-taboo‘ that I was breaking when I casually mentioned my occasional outburst at a senior management, leadership course. My casual revelation during a group discussion, precipitated a wave of quiet, concerned looks and corridor hugs.
Sensitive men had all the fun it seemed.
I believe that most doctors cry, male and female, the reserved and the pathological, although we would all prefer not to. It’s a painful business, unwittingly connecting with the anguish and the suffering that we witness. The public, whom we serve, might expect us to be moved by their experiences, empathetic and understanding, and also remain placid and calculating. The discomfort of seeing your medical professional crying over your loss, or your impending demise, was not really what anyone wanted. Warmth and empathy were rarely expressed and on ICU, regarded with suspicion.
I once spontaneously kissed a brave, paralysed, spinal-injury patient who returned unannounced to the unit to deliver a box of chocolates. Not a Trumpesque smooch on the the lips, just a peck on the cheek. Even so, the nursing staff appeared distinctly uncomfortable with my genuine delight at seeing her. I hadn’t planned to react thus, but I was so surprised and moved to see her cheerful face, so full of vigour and life that it seemed only natural. The more conventional show of joy, the hug, was not that easy to accomplish with someone in a wheelchair. If you were not careful, you could find yourself shoving their face into your groin as you semi-bend over and hug their head. Even I had limits to my interactions.
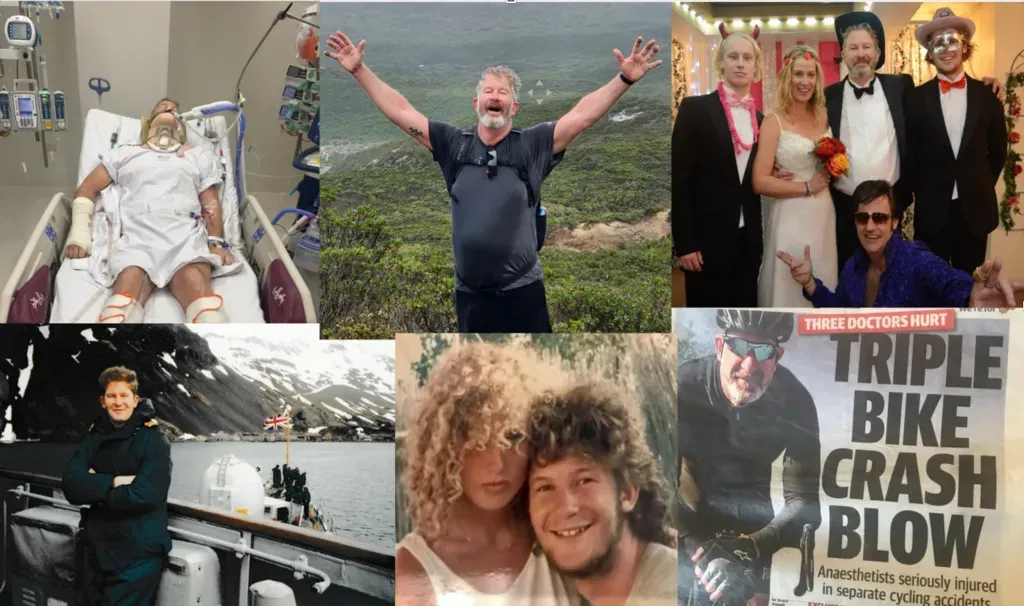
I’d known the lady for three months, from her near-death-admission, to her triumphant, admittedly wheeled, departure. When I think of her fortitude and her injuries now, having broken my own neck and back and walked out of hospital seven weeks later, it is hard to contemplate such human spirit. I don’t think that I would ever have spoken civilly to anyone ever again if I’d have been paralysed. I’d have gone for the Lieutenant Dan, Forrest Gump version, raging against life and smoking huge amounts of weed. Of course “Lootenant Dan” becomes wealthy, regains his will to live and even walks again on his “magic titanium legs”. Back in the real world, my legs hadn’t been blown off by a land-mine and worked only a week after the crash, so I wasn’t exactly Stephen Hawking either.
Shedding tears, connecting with other’s pain, doesn’t necessarily make you a better doctor. It might actually render you ineffective in a crisis or break you in the longer-term. A brain surgeon, an ED physician, an executive nursing officer, as leaders, may not have the luxury to be so self-indulgent. It’s not cold-hearted to become accustomed to death and suffering, if that is your normal daily routine. For me, there might be 20 patients on the Intensive Care Unit. If bed one was the helmet-less motorcyclist who had left his testicles on the handlebars of his Harley as he crashed and broke the world long jump record, there was still 19 other patients to care for, so we moved on. One of my bosses used to reverse the order in which we saw the patients, start at no. 20 instead of one, each alternate day. I could only ever remember about half the patients by name, so that worked well for me. Whichever end you started, after two hours of concentration, everyone was drained. You most certainly couldn’t emotionally care for everyone, solve their complex, life-threatening medical condition and recall who asked for the “Berry Hibiscus Refresher” on the day’s coffee order.
Despite all that training and those learned professional strategies, you could still be caught out. There would be a sudden, unexpected lump in the throat and a strange hiccup instead of a steady intake of breath, like suddenly realising you are going to be sick. There would always be a patient that triggered the gut-reaction but not in isolation. Such a dramatic reversal of mood could be precipitated by up-all-night-fatigue, or a patient’s extraordinarily tragic plight, but often a combination of both. The more experienced I became, the less likely it was that I would be shocked or surprised, but the rare times I was truly moved, the experience was even more intense and draining.
I read that each different area of medicine tugs upon their own unique heart-string. In the emergency department, if tragedy is to strike, patients normally die within the first two hours of their arrival. Thus the principal emotion is shock, often made worse by the tendency for patients to be younger and previously well. On the contrary, patients who die after weeks in hospital, have fostered relationships with staff. There is more sadness and a sense of loss for doctors and nurses alike, often shared with relatives whom they have come to know. In Intensive Care Units, patients have about a 20 percent overall chance of dying, or much higher depending on what is wrong with them. Hence it is not a shock when people die, but it is often after a long, courageous struggle and a period of shared relations and friendship.
I used to smile knowingly to myself when chatting to relatives who would optimistically say, “They’re a real fighter, you know Doc.” That phrase invariably condemned the patient to a drawn out and painful death. “They’ll just give up and die, Doc.” That would have been much easier to witness and less traumatic, but it never happened. The human spirit and a bloody-minded refusal to let this sweet life go, just didn’t allow it.